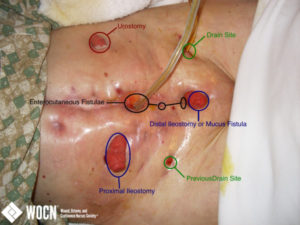
COMPLEX ABDOMEN WITH FISTULAE (LABELED)

Surgical History: This 71 year-old female presented with SBO 3 weeks after radical cystectomy and ileal conduit formation. After failing medical management, patient underwent ex-lap and small bowel resection for obstruction secondary to an adhesive band of omentum and stricture with ulceration. Five days later, patient had enteric contents draining from her wound. Patient was re-explored and an anastamotic dehiscence was found. Patient subsequently underwent a series of operations in an attempt to control newly developing leaks (several in areas where serosal tears had been repaired). Patient continued to develop leaks despite proximal diversion of the bowel. Eventually her visceral mass was no longer dissectible, and drains were left in place. Patient’s nutrition has been maintained on TPN. Wound and Ostomy Management: Both the proximal and distal ileostomies only put out a small amount of mucus. The superior and inferior fistulae are high output (the middle fistula only has a small amount of output). Both of the drain sites are putting out small bowel drainage as well. Currently, we are getting three days wear time, even with the patient getting out of bed. We are using pediatric urostomy pouches on both drain sites and the superior and inferior fistulae (and the distal ileostomy because it is so close to the inferior fistula). We are placing a neonatal pouch over the middle fistula, then a standard fecal pouch over the proximal ileostomy and a standard urostomy pouch over the urostomy. We had difficulty using standard fistula pouches because the angle never seemed to be right for the pouches to flow into a bedside drainage bag and even with proper removal, they often caused skin breakdown.
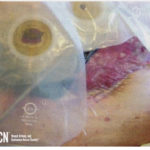
ABDOMINAL WOUND WITH STSG AND FISTULAE

Background: This 9 y.o. female was brought in by Life Flight as a LVI trauma direct-to-OR admission. Patient was a rear-seat restrained passenger in a high-speed side impact MVC. Initial abdominal injuries include: traumatic abdominal hernia, aortic dissection, descending colon perforation, small bowel bucket injury, and ascending colon deserosalizing injury. Patient had an open abdomen for an extended period of time and developed multiple small bowel fistulae. Approximately 3 months after initial injury a STSG was used to close the remainder of the surgical wound around the fistulae. Patient’s nutrition is being managed with TPN. Patient is also on IV fluid replacement based on fistula output. Photo was taken approximately one year from initial injury. Wound and Ostomy Management: The fistula output is completely liquid and runs between 800mL and 3,000mL per day (depending on PO intake). Currently, we are using a medium wound pouch with catheter to continuous suction. The open skin around the fistulae was treated with ostomy powder followed by standard barrier spray followed by a cyanoacrylate-based skin prep. Barrier rings are then used to fill creases and create a flat pouching surface.
ENTEROCUTANEOUS STOMATIZED FISTULA

Present in abdominal wound.
ENTEROCUTANEOUS FISTULAS

Multiple fistula sites in abdominal wound.
POUCHING OF ENTEROCUTANEOUS FISTULAE
Use of pouching and negative pressure wound therapy.
ENTEROCUTANEOUS FISTULA WITH NEGATIVE PRESSURE WOUND THERAPY MANAGEMENT

One stomatized and one poorly visible fistula, isolated; remainder of wound managed with NPWT.
ENTEROCUTANEOUS FISTULAE

Open abdominal surgical wound, ventral hernia, with multiple fistulae
SURGICAL WOUND COMPLICATED BY ENTEROCUTANEOUS STOMATIZED FISTULA

Stomatized fistula in abdominal surgical wound.
DEHISCED SURGICAL WOUND WITH ENTEROCUTANEOUS STOMATIZED FISTULAE

Present in abdominal surgical wound.